 Sever's disease, also known as calcaneal apophysitis, is a common cause of heel pain in growing children and adolescents, particularly those involved in sports. It occurs when the growth plate in the heel becomes inflamed due to repetitive stress and overuse. This condition typically affects children between the ages of eight and 14, coinciding with periods of rapid growth. Patients with calcaneal apophysitis often experience pain and tenderness in the heel, which can worsen with physical activity and improve with rest. The pain is usually located at the back of the heel and can be accompanied by swelling and difficulty while walking. Treatment focuses on reducing pain and inflammation, and rest is commonly suggested. Stretching exercises, wearing proper footwear, and orthotic inserts can also help to alleviate symptoms. If your child is complaining of heel pain that persists, it is suggested that you visit a podiatrist for a thorough evaluation and tailored treatment plan.
Sever's disease, also known as calcaneal apophysitis, is a common cause of heel pain in growing children and adolescents, particularly those involved in sports. It occurs when the growth plate in the heel becomes inflamed due to repetitive stress and overuse. This condition typically affects children between the ages of eight and 14, coinciding with periods of rapid growth. Patients with calcaneal apophysitis often experience pain and tenderness in the heel, which can worsen with physical activity and improve with rest. The pain is usually located at the back of the heel and can be accompanied by swelling and difficulty while walking. Treatment focuses on reducing pain and inflammation, and rest is commonly suggested. Stretching exercises, wearing proper footwear, and orthotic inserts can also help to alleviate symptoms. If your child is complaining of heel pain that persists, it is suggested that you visit a podiatrist for a thorough evaluation and tailored treatment plan.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see one of our podiatrists from InStride Family Foot Care. Our doctors can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Concord, Charlotte, and Salisbury, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.




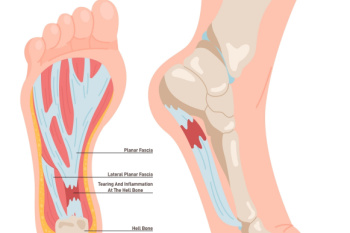 Plantar fasciitis
Plantar fasciitis



 Rheumatoid arthritis
Rheumatoid arthritis